
Many families are unfamiliar with Palliative Care and often confuse the services for hospice or end of life care. However, palliative care is so much more. Palliative Care is a specialized system of care aimed at improving quality of life for patients and their families living with a serious medical condition. The palliative care team (sometimes abbreviated as PaCT) works alongside your other medical teams to focus on supporting individuals and their family during times of stress. This may include times of change, discomfort or pain, or other emotional needs. The palliative care team helps you think about what is most important to you and coordinate care with your other teams to ensure that your medical care aligns with your goals and values. Think of palliative care as another layer of support in your medical team.
It’s important to know that palliative care can be appropriate at any age or stage of Duchenne and Becker. There is no such thing as “too early” for palliative care. Building rapport with the palliative care team over time leads to optimal support during challenging experiences such as periods of change, difficult decisions and more. Individuals and their families face many healthcare decisions during the course of their lives, such as:
- Should the individual start a certain treatment?
- Should the individual pursue a certain surgery?
- What about enrolling in a clinical trial?
Each individual and their family navigates these decisions differently. There is not one right answer for what a person “should” do. Palliative care teams recognize that each patient is unique. They help each patient and family think about what is important to them, while aiding in certain decisions that are most in line with their personal goals and values.
Getting to know the palliative care team over time helps build trust so that you feel comfortable having these conversations with someone who knows and understands your child and family. Beyond supportive decision making, other examples of palliative care support include: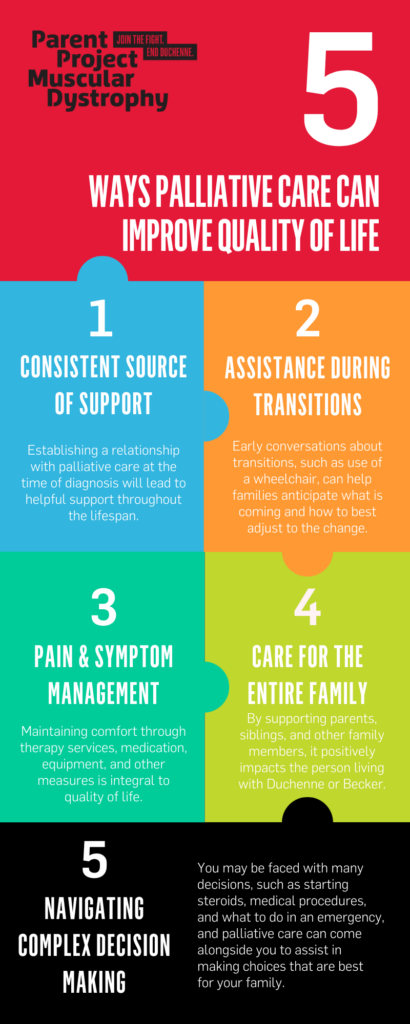
- Pain management
- Mental health issues such as anxiety or depression
- Gastrointestinal symptoms such as nausea, vomiting, constipation and abdominal pain
- Skin issues such as wounds or rashes
- Sleep difficulties
Palliative care services may be needed more often as patients with Duchenne and Becker get older. The palliative care team can work alongside your neuromuscular team as symptom management experts, to evaluate and treat these symptoms, especially as they become more difficult or severe.
While not the sole purpose, some palliative care clinicians are also experts in providing hospice and end-of-life care. Hospice care is a system of end-of-life care for patients who are expected to live six months or less. Like palliative care, hospice also focuses on symptom management and quality of life. More information about the difference between palliative care and hospice can be found here.
In summary, palliative care reaches far beyond end-of-life decision making. It is support throughout one’s life to ensure one’s values are honored in every aspect. If you haven’t met with a palliative care team during your neuromuscular visit, be sure to ask at your next visit. Each of PPMD’s Certified Duchenne Care Centers have access to palliative care services for their patients.
WEBINAR RECORDING
PPMD recently hosted a webinar to provide more information about how palliative care can support individuals and their family.



 by: Parent Project Muscular Dystrophy
by: Parent Project Muscular Dystrophy

