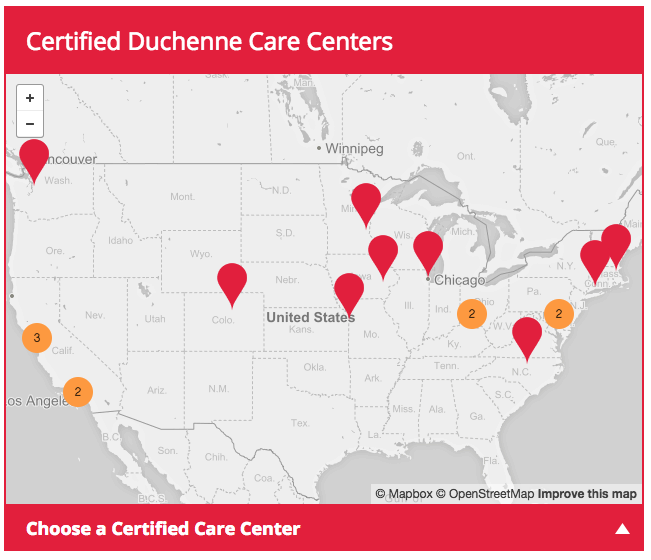
PPMD’s Certified Duchenne Care Center (CDCC) Program was developed to make comprehensive Duchenne care and services, provided in agreement with the CDC Care Considerations, available and accessible to as many families as possible, and to strengthen clinical trial results by decreasing variability in care among clinical trial subjects.
The CDCC network has now grown to 18 incredible centers across the United States, includes more than 500 medical providers, and serves more than 2,500 patients and their families. These 18 centers are sites to 39 clinical trials, enrolling more than 1,142 patients, who are either currently enrolled or in active recruitment (these are averages based the number of subjects and the number of sites for each trial).

2018 CDCC Happenings
PPMD was extremely happy to host the first Duchenne specific medical conference. The Duchenne Clinician Conference was held January 24-26, 2018 educating more than 120 medical and industry partners on the sub-specialty specific recommendation for Duchenne care and services that are included in the updated Care Considerations. Information was provided across all subspecialty areas with elements of care in each area specified across the life span. In addition there were deeper dives into several specific areas (i.e., palliative care, transition, etc.). We will be hosting the 2nd Duchenne Clinician Conference, January 23-25, 2019, with more a more in depth look into key areas of interest. The agenda will be out soon, so please let your medical providers know!
 Working with both the NIH and the Shirley Ryan Ability Lab, PPMD was able to convene a meeting on Contractures in Duchenne and Other Neuromuscular Conditions (April 19-20, 2018). Gathering expertise across the pathophysiology, evaluation, prevention and management of contractures in several diagnoses has resulted in slight amended evidence based recommendations for PT’s and families. A published summary, as well as new resources for our community, will soon be released.
Working with both the NIH and the Shirley Ryan Ability Lab, PPMD was able to convene a meeting on Contractures in Duchenne and Other Neuromuscular Conditions (April 19-20, 2018). Gathering expertise across the pathophysiology, evaluation, prevention and management of contractures in several diagnoses has resulted in slight amended evidence based recommendations for PT’s and families. A published summary, as well as new resources for our community, will soon be released.
The PPMD Annual Conference included families, industry and more than 60 non-industry medical providers. Sessions discussing cardiac care across the diagnosis, participation in clinical trials, and stage-specific care breakouts provided opportunities for discussion around all areas of Duchenne care. The larger sessions were recorded and are available on the PPMD website. The care breakouts were not recorded but, if you were unable to join (or if you were!) and have questions about the content the speaker(s) covered, please let us know.
Bi-Annual Report of Each Center – August 2018
The table below describes the bi-annual report of each center.
The Monitoring Process
The CDCC is monitored by the CDCC Certification Committee – a steering committee of 19 individuals who represent several areas of neuromuscular subspecialty care, parents, industry and PPMD –review each application and site visit summary, and make suggestions/recommendations regarding certification. If center issues arise, this committee gathers to discuss the issue and potential solutions, and to discuss these solutions with the center. It is then the responsibility of the committee to follow up on the solution, to make sure that that recommendations are followed and that the issue is resolved.
Your Input is Vital
The Clinical Experiences surveys that we ask you to complete each year, let the CDCC Certification Committee know what elements of care and what services you are receiving, and what you like and what you do not like about the care and services at your center. We put all of your responses together each year and give those back to the centers.
The Certification Committee takes a deeper dive into any issues or concerns that are raised, and the centers use your feedback to continuously improve the care and services that you are receiving at your center. Completing the Clinical Experiences Survey annually is vital to the continuous improvement of the centers and our program.
Complete the Clinical Experiences Survey >PPMD Is Dedicated to Improving the Care of Every Single Person Living with Duchenne
In addition to the expertise offered by the expert clinicians at our CDCCs, PPMD is available to offer medical guidance when needed, referral and connection to appropriate medical personal and genetic counseling to patients, parents, and providers. We are available when you need us and will do our very best to make sure that you get the information and assistance that you need.
PPMD is extremely proud of what the CDCC Program has been able to accomplish in 3 years, but we have not done it alone. With the help of compassionate and dedicated clinicians and families, we have initiated a program that we hope will work to provide everything that our Duchenne community will need for decades to come.
Reminders for Parents in Emergency Situations:
If you are headed to the emergency room or the hospital, please remember:
- Take the PPMD emergency card with you
- Take a copy of the summary of your last neuromuscular visit with you or a brief 1 page summary of your/your child’s care
- Download, and keep handy, the PPMD mobile app
- Take any equipment that you use at home (cough assist, BiPAP, etc.) and medications that you take, with you
- Take a copy of your last ECG with you. (All people living with Duchenne have an abnormal baseline ECG. Providing the emergency team with your baseline heart rate and rhythm will help them to know if anything has changed.)
- Keep the information regarding oxygen use and appropriate anesthesia available for you and the emergency room staff
- Call your neuromuscular team and let them know what is happening
- Be sure that your neuromuscular team is talking with the emergency staff and are guiding your care
- If you/your child has developed an “emergency care plan,” take that as well
- If you need assistance, call the PPMD office at 800-714-5437. If the office is closed, Kathi Kinnett is available at kathi@parentprojectmd.org or 513-260-4004.


 by: Parent Project Muscular Dystrophy
by: Parent Project Muscular Dystrophy