Your Rehabilitation Team
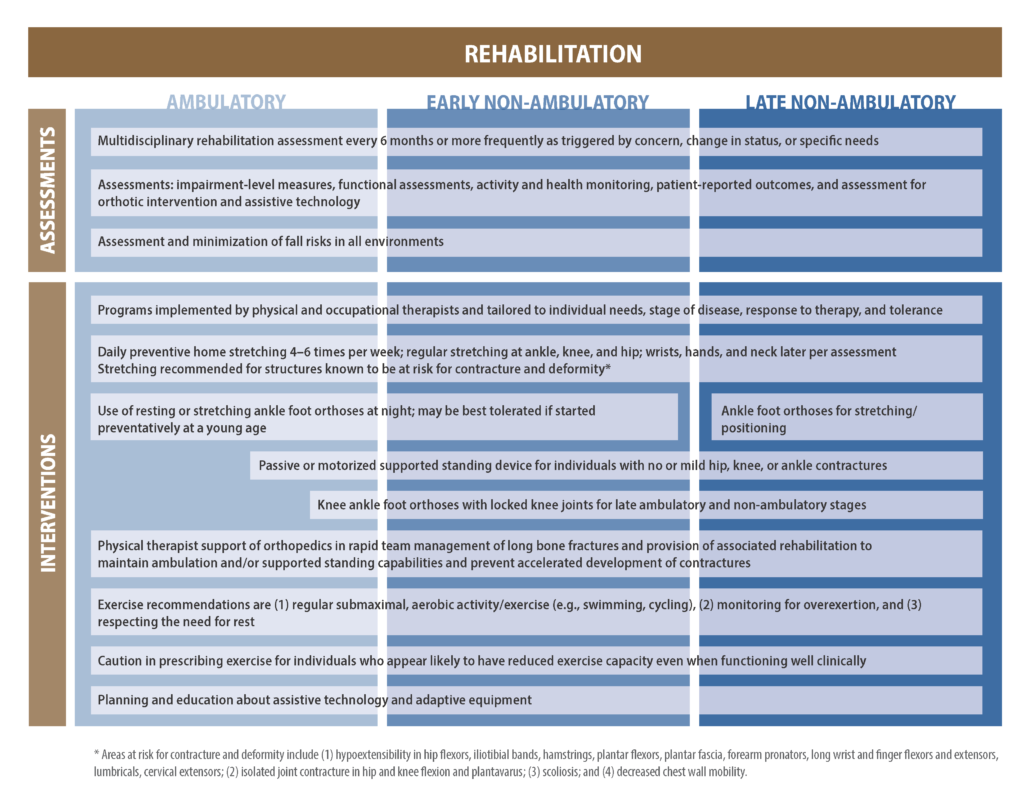
Rehabilitation teams should include physicians, physical and occupational therapists, speech language pathologists, orthotists and providers of durable medical equipment. This team works to collaborate with the other subspecialty members of the Duchenne care team (i.e., neuromuscular specialist, cardiologist, pulmonologist, endocrinologists, etc.).
Physical Therapy
Physical therapy (PT) will be an important part of life from the time of the Duchenne diagnosis. It is important that you have specialized physical therapy evaluations every 4-6 months. This way, any and all changes can be tracked overtime and needs can be addressed quickly.
Physical therapists play an important role in:
- Minimizing contractures by introducing regular stretching into your daily routine
- Maintaining function and adapting to any loss of function
- Monitoring function over time through standard tests and measures
- Assessing for and managing compromised skin integrity
- Preventing and managing pain
- Prescribing exercise and supervising safe physical activity (i.e. low load, low resistance exercise)
- Recommending mobility devices, adaptive seating, and other equipment
- Rehabilitation after injury or fracture
Physical therapy is different in Duchenne than in other situations. In other diagnoses, PT can help increase range of motion, strength, and function; in Duchenne, the goal of therapy is to preserve range of motion (the flexibility of a joint), strength, and function. PPMD videos will help your PT to provide the best therapy for you/your child.
Physical Therapy’s Role in the Care Team
Your physical therapist should work closely with your neuromuscular specialist, physical medicine & rehabilitation (PM&R) physicians, occupational therapists, speech-language pathologists, or any other providers who make up your rehabilitation team. This team will focus on your individual goals and lifestyle and provide appropriate care. Physical therapists play a major role in obtaining appropriate adaptive seating and other types of equipment. They can also work with your family and help advocate on parent’s behalf to insurance companies. Physical therapy will be involved in the rehabilitation after an injury or fracture to regain function and ambulation. You should have a thorough physical therapy evaluation (strength, function and range of motion of the hips, knees, ankles, shoulders, elbows and wrists) at least every 4-6 months. These measurements should be tracked longitudinally so that indications of muscle weakness or joint tightness are found, and treated, early. Such evaluations can also indicate when some forms of equipment may be needed in the future.
Skeletal muscle attaches to the tendons and joints of the body. In Duchenne, skeletal muscle is replaced by fat and scar tissue. The fat and scar tissue that replace the skeletal muscle are less flexible. This loss of flexibility in the muscle can lead to loss of range of motion at joints limiting how much a joint can move. Loss of joint mobility in combination with muscle weakness and less active movement can lead to a contracture or a fixed position of a joint. In Duchenne, an area of tightness commonly seen is at the ankle with a result of loss of flexibility of the Achilles tendon or heel cord.
There is still a lot to learn about contractures in Duchenne, however keeping the joint mobile within the available range of motion is important and has many benefits (see below). You should see a PT for an evaluation at least every 4-6 months. Stretching regularly and wearing night braces (feet and ankles) will help the joints stay mobile. Your PT team will also monitor the strength, function and range of motion of all of your joints at each visit. This evaluation should include shoulders, elbows, wrists, fingers, hips, knees and ankles). The results of this evaluation will help them to know when joints are becoming tighter so that they can make recommendations specific to you for appropriate stretches and/or braces for these joints.
Non-Surgical Contracture Management
Working to prevent contractures proactively (before they occur) is always best. Contractures are not always preventable. If they do occur, there are ways to manage contractures and maximize the function of the joint. PPMD worked with a team of expert Physical Therapists (PTs) to develop an easy to follow Range of Motion handout (download) for parents and physical therapists. This handout summarizes the current physical therapy guidelines explained below.
Download Range of Motion Guide >Stretching
Stretching should be a part of your daily routine and should be guided by your physical therapist. Regular stretching of joints including the shoulder, elbow, wrist, ankle, knee, and hip should begin early and continue through adulthood. Potential benefits of stretching may include:
- Temporary improvement in blood flow to the muscle
- Decrease report of discomfort
- A feeling of wellbeing
- Temporary increase in tolerance to stretch
- Temporary decrease in muscle stiffness
- Continued movement through the joint’s full available range of motion
Watch: Video Demonstrations
To view a collection of videos demonstrating stretching routines in people living with Duchenne of all ages, please visit our PT video series page.
Bracing
Bracing helps to keep the joints in alignment and maintain flexibility and function of the joint by providing a long (maintained) stretch. Braces can be used on the lower limbs (ankle-foot orthosis (AFO) and knee-ankle-foot orthosis (KAFO), the wrists, and the hands. Braces are often made of plastic and are made specifically to fit an individual, custom fitted by an experienced occupational therapist or orthotist.
As we mentioned above, in Duchenne, tightness first develops in the ankles, due to the shortening of the calf muscle and pull on the Achilles tendon. Wearing braces at night (“night splints” or “moon boots”) enable the joints of the ankle and feet to be stretched for several hours. Most children are encouraged to start to wear night splints at, or near, the time of diagnosis to improve tolerance and wear time. These braces are called “AFO’s” (ankle, foot orthoses). The specific type of brace that you will need will be ordered by your physical therapy team. Wearing splints of this type are not recommended during the day, as they have a tendency to increase falls and increase the demand on the quadriceps (thigh) muscle. It is important that you are evaluated by a PT who is familiar with Duchenne.
PPMD has created videos demonstrating how to properly apply AFOs to children and adults with Duchenne. To view these videos, please visit our PT video series page.
View Stretching Videos >Serial Casting
 Serial casting refers to a process of applying a series of rigid casts (typically plaster) over an individual’s joint (most often used for heel cords at the ankle). The casts are used to slowly (with frequent cast changes over several weeks) increase range of motion at a specific joint. The joint is stretched “slightly” further with each new cast placement, which is typically 1-2 times per week. This procedure is not done at all centers, and should only be done at centers familiar with both the procedure and Duchenne. Careful monitoring by an PT with experience in serial casting and Duchenne is critical for success.
Serial casting refers to a process of applying a series of rigid casts (typically plaster) over an individual’s joint (most often used for heel cords at the ankle). The casts are used to slowly (with frequent cast changes over several weeks) increase range of motion at a specific joint. The joint is stretched “slightly” further with each new cast placement, which is typically 1-2 times per week. This procedure is not done at all centers, and should only be done at centers familiar with both the procedure and Duchenne. Careful monitoring by an PT with experience in serial casting and Duchenne is critical for success.
Positioning
As mobility devices become necessary, these, too, will need to be evaluated by your physical therapy team. It is important that the device is used safely (wear your seat belt always and chest strap, if needed) and that the device offers optimal support and proper positioning. Following the advice of your physical therapist regarding when specific mobility devices are needed, is important. Your physical therapy team will help you to access the devices most appropriate for optimizing your function and quality of life.
Use wheelchair inserts and support
Bolsters, rolls, or pillows can be used to position or support a body part in a good alignment. When individuals are spending increasing amounts of time in a seated position or lying down, muscles and joints become stiff more quickly. It is important to be sure they are in good position to help maintain their range of motion and comfort. Ideal seated positions include:
- Both feet flat on the floor or footrest (or box step for younger boys), with hips and knees at a 90-degree position and back and pelvis aligned with hips
- Avoid long periods of time with legs in a frog position (splayed out). Knees should be in line with feet & hips.
- During growth, changing the dimensions of the chair helps maintain the best upright posture without having to lean.
Subtle changes in wheelchair posture may indicate possible changes in the spine. Wheelchairs should have inserts on it so you are able sit upright and keep all parts of your body supported and in the proper position. If you are not having spinal surgery and your back pain is getting worse, a back brace may help.
For a detailed look at posture and seating, refer to our Mobility & Accessibility page. PPMD created a series of videos demonstrating safety and benefits of various wheelchair positions, which can be found on the PT video series page.
View Stretching Videos >Standing devices
Standers are custom-fitted equipment designed to help an individual stand up for a prolonged amount of time. Standers could be considered in children who are unable to stand by themselves, have difficulty standing, or have lost the ability to walk. There are a few options for standing devices:
- Sit-to-stand standers: allow ta person to go from sitting to a standing position
- Supine standers: provide support along the back of the body; the child lies down and then is brought to standing
- Wheelchairs that transition to standing
For a detailed look at standers, refer to our Mobility & Accessibility page.
Safety
Preventing falls will go a long way to helping to maintain ambulation. Inside, making sure areas are as free from clutter, slippery surfaces or fall hazards, as possible, is helpful. Outside, paying attention to uneven surfaces and slippery surfaces can also help to prevent falls. And, again, if you are on a mobility device, wear your seat belt!
Physical Activity and Exercise
Physical therapists have an important role in prescribing, monitoring and guiding exercise. Aerobic exercise should be low or no impact, with minimal resistance. Swimming is generally the best exercise as there is less stress on postural muscles in an aquatic environment. It is important not to become over fatigued and to allow for rest periods. Talk to your physical therapist and rehabilitation team about what is safe.
Additional Daily Reminders
In addition to daily stretching and night-time bracing, there are a number of smaller items you should remember to incorporate into your daily routine to help preserve flexibility, strength, and function of your skeletal muscles, including:
- Sitting up straight with good support
- Keeping knees together and feet supported
- Moving hands and wrists often
- Keeping your tongue in your mouth
- Exercising jaw muscles
- Staying safe
- Remembering to rest when you need to
Watch: Head, Shoulders, Knees, and Toes
Additional Resources
- PT Management Document (download): This article details the importance of physical therapy in treating Duchenne.
- Important Aspects of Physical Therapy (review): Presented by Helen Posselt at PPMD’s 2010 Connect Conference.
- Templates for developing letters of medical necessity and letters of appeal